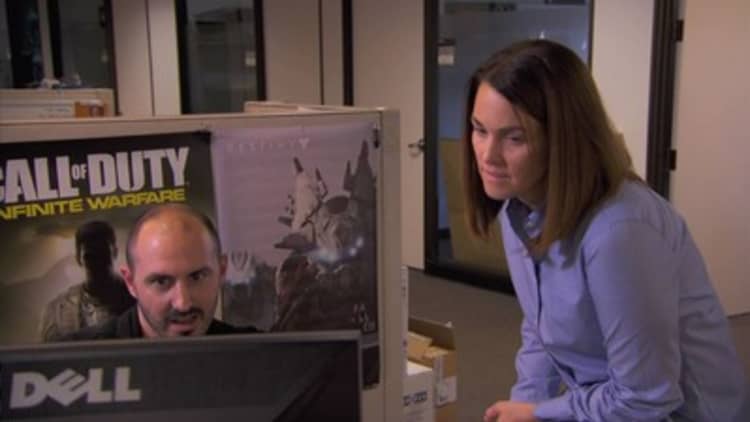
Gina Hope loves her job helping market games like "Call of Duty," at Activision Blizzard in Los Angeles. Her health insurance was another thing.
"I have a son with special needs," Hope explained. "We don't want to be switching from provider to provider, because it's a learning process every time somebody new comes into the picture."
Her child's provider was out of network and for years it has meant she spent thousands of dollars for his care out of pocket.
When Activision Blizzard switched to a start-up benefits manager called Collective Health for 2016, she was skeptical. She checked was to see if her son's provider was covered. He wasn't. She mentioned it to her colleagues in Human Resources, not expecting anything to happen, but then things changed.
"The next thing I know, they had signed up my son's provider and brought him in network for me without me even asking — without me making a phone call," Hope said. "And this year, it saved us $17,000."
That kind of service is why Activision's H.R. chief took a chance on the start-up.
"We're not a huge organization," said Milt Ezzard, the company's senior director of global benefits. "We don't have all of the muscle power like a Microsoft would have to push a (health insurance) carrier around to do things in a way that makes sense to us. But I have a mentality that we deserve that kind of treatment."
The founders of San Francisco-based Collective Health launched the firm in 2015 out of their own frustration with the way their health insurance benefits worked.
"I'm a doctor who did a PhD in political economy," said Dr. Rajaie Batniji, one of the firm's co-founders, "and frankly I'm very confused when I try to access the (health-care) system."
A data-driven approach
While other health insurance upstarts like Oscar Health targeted the new Obamacare consumer market, Collective Health has focused on self-insured employers who represent the largest share of the health-care market. Most mid- and large-size firms pay directly for health costs and hire traditional commercial insurers to negotiate provider networks and administer benefits.
"Employers are the ones who can actually move the fastest to adopt innovation, to adopt change, and they've got the best incentive to do that," said Batniji.
The startup employs 250 workers, and has raised more than $100 million in backing from investors that include Founders Fund and Google Ventures.
Collective Health's approach is data-driven, and it starts with a streamlined platform that lets employees see all of their health-benefit choices, bills and information about deductibles and payments in one place.
"We aren't encumbered by the legacy system that all those big carriers have," explained Batniji. "We have the luxury of starting from scratch and creating a system that's built on modern software... to create that member experience that feels like the best of consumer tech products."
They also have the luxury of concentrating on the service part of the business, since Collective Health doesn't get involved in negotiating provider contracts. Instead, it pays larger insurers like Blue Cross to use their medical networks.
That allows the Collective health team to focus on leveraging claims information to help companies like Activision Blizzard understand how well their health benefits and wellness benefits are working, and anticipate what kind of care employees will need.
"If we get somebody who we recognize from our claims data that looks like they're going to have a major surgery coming up, we can direct them to get a second opinion, and make sure they're plugged into a care management solution," said Batniji.
More from Modern Medicine:
New prostate cancer tests aim to reduce the death rate
Antibiotics are becoming the David to the Goliath of 'Superbug' infections
Writing a prescription ... for a dose of electricity
Being proactive pays
Like a lot of large employers, Activision has dozens of wellness programs to help their workers get the most out of their benefits, but the company's old insurer wasn't as proactive about helping employees make the most out of those benefits.
"Our healthy pregnancy utilization is triple what it was under our conventional carrier's watch, so we know that moms are engaging and tracking their pregnancy," said Activision's Ezzard. While that might seem like it would cause bigger expenses, he says it actually pays off in the long run.
"I know the costs of members that are continually engaged is actually lower per year by a cost of about $800 per member," Ezzard said.
For Gina Hope, the switch to Collective Health is certainly paying off.
"I've never raved about my insurance, previously," she said. "But they treated me like a person. I wasn't just a box to check."
Activision is renewing with Collective Health for 2017. It's a big vote of confidence for the start-up, which expects to double its employer business next year, bringing the number of members covered to more than 70,000 people.





