California's Obamacare marketplace said Thursday it will require insurers submit two sets of proposed prices for health plans next year because of continued uncertainty over whether the federal government will continue reimbursing insurers for crucial subsidies.
One set of rates would be used if there is not a clear sign that the Trump administration and Congress will fund the subsidies through 2018, which would reduce revenue to insurers.
The other set of rates would assume that the subsidies, known as cost-sharing reductions, are continued throughout 2018.
Covered California recently estimated that premiums for so-called silver plans would rise by 16.6 percent beyond the normal premium hike if the federal government ceased the CSRs. Allowing insurers to submit two sets of rates could make it easier for Covered California to retain insurers on the marketplace.
The CSRs reimburse insurers for subsidies that Obamacare legally requires them to offer to low-income customers who enroll in silver plans — the type of plan that covers an average of 70 percent of the health costs of enrollees.
The subsidies reduce the amount such customers have to pay in out-of-pocket costs when they go to the doctor or hospital, are prescribed medications, or receive other health services. The rates are worth an estimated $7 billion to insurers nationally this year.
The announcement comes amid uncertainty over whether Congress and the Trump administration will cease paying the CSRs.
The Republican-controlled House of Representatives several years ago sued the Obama administration, saying the CSRs should not be paid to insurers because Congress never appropriated the money for them.
But the federal government kept paying insurers for the CSRs as the case continued in a federal court, and even after a judge ruled in the House's favor. The judge's decision was stayed pending an appeal by the Obama administration.
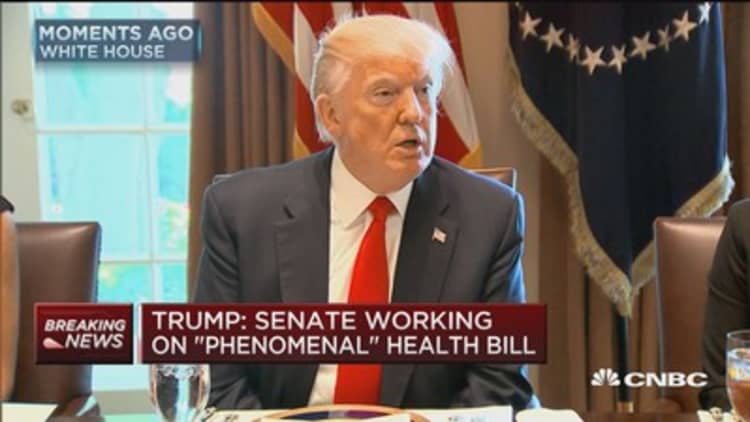
The inauguration in January of President Donald Trump, an avowed opponent of Obamacare, raised the possibility that he would order the Justice Department to drop defense of the court case, and stop paying the CSRs.
But instead, the administration and the House have agreed to stay the appeal of the case, while they discuss a possible resolution of the case.
That agreement, on its face, may seem perplexing, because both Trump and House Republicans have long campaigned against Obamacare. But the agreement reflects concerns that eliminating the CSRs would harm insurance companies, and then would hit consumers' pocketbooks when insurers raised prices in reaction. This could possibly lead to political backlash for Republicans.
However, Trump has publicly said he might cease funding the CSRs. His proposed budget for next year calls for continuing to fund the subsidies until the court case is resolved.
Watch: Obamacare architect offers prescription for uncertainty



