In January 2018, a search kicked off for an executive who could help three gigantic companies -- Amazon, Berkshire Hathaway and J.P. Morgan -- rethink one of their biggest cost drivers: Health care.
As of 2019, the average total cost of employer-provided health coverage passed more than $20,000 for a family plan and are rising around 5% per year.
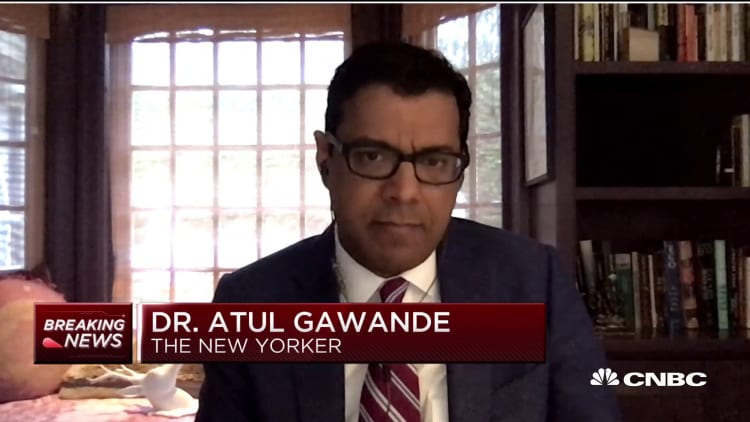
So Haven had come along at a good time and it was attempting to solve some very real problems, particularly given that employers purchase health care for almost half of all Americans. CEO Dr. Atul Gawande, a visionary physician and writer, would have the weight of three billionaire company leaders -- Amazon's Jeff Bezos, Berkshire's Warren Buffett and J.P. Morgan's Jamie Dimon behind him.
But after a little more than two years on the job, Gawande this week announced he would be stepping aside from Haven to focus on other areas, including on the Covid-19 crisis, after two years on the job. The company is now looking for a new CEO, while its COO -- Mitch Hetses, a longtime CVS executive - takes on day-to-day operations.
Despite his departure, many health industry insiders agree that there's still a path forward for Haven. The key will be for the executive teams to rally behind this person in a big way, and for this new recruit to bring benefits into lockstep with their plans. Get it right, and there's still big upside.
"Innovative employers, partnered with the best providers, are most empowered to fix United States health care," said Jonathan Slotkin, chief medical officer of Contigo Health, an employer health-focused company that was formed inside Premier. "It really will take a partnership of the providers who deliver care and the employers who pay for that care," he said.
Here are the three areas that experts told CNBC are still likely to be the target of Haven, or any other employer-focused group trying to change health care:
- Forging direct deals with hospitals
- Lowering pharmacy costs
- Better access to primary care
Deals with hospitals
Elizabeth Mitchell runs the Pacific Business Group on Health, which works with large employers to test out new ways to bring down health care costs, and has been a believer in Haven's potential since the beginning. In her view, it's "hard but not impossible" to shake up employer-sponsored health care without jeopardizing quality.
She recognizes that it's a big challenge to change up employee health benefits in the midst of a pandemic, but still sees a viable path forward for Haven.
First, she believes Haven should hire a new executive who has experience with benefits and can help the employers understand how the system really works. Bringing on a newcomer to the space would likely set the company back further still.
Mitchell would expect Haven to delve deeper into direct contracting. Large employers like Boeing, General Motors and Walmart have been striking deals for years, often referred to as "centers of excellence" programs, with a provider organization. That way, they can ensure that their employees will be seen by higher-quality providers, and they'll be far less likely to pay for unnecessary care.
Slotkin, with Contigo Health, has been highly involved with an initiative like that in his other role treating patients as a neurosurgeon at Geisinger Health. When an employee is diagnosed as needing spine surgery, Walmart, at its own expense, will send employees to Geisinger to get a second opinion from a doctor who isn't financially incentivized to recommend procedures. Many, in fact, do not.
The company's Centers of Excellence program, which requires its employees to use a curated list of hospitals for some surgeries, has been in place for about seven years. (It was optional until 2018.)
These sorts of programs tend to work best when the executives behind these companies are totally engaged, experts say.
"To sidestep payers, you need a business imperative and you need the support of the CEO," said Gillian Printon, the head of national accounts at Centivo, a company that is helping employers navigate health care costs. The reason for that is some employees might resist a so-called "narrower network," preferring instead to see a medical provider that they're loyal to.
"It can feel to some people like it's paternalistic or choice limiting," said Dr. Sachin Jain, an adjunct professor at Stanford Medicine and a former health insurance executive.
Printon said that there's another challenge: To get these direct contracting programs to work, it often requires that the employer have a large concentration of workers in a specific geographic location. For Haven, that might mean bringing on other employers to its consortium that have more of an overlap with the current distribution for J.P. Morgan, Amazon and Berkshire Hathaway.
"Ultimately, these are hard trade-offs to make in a system of interdependencies," said Jain.
Forcing change
Other areas that Haven will likely try to tackle are pharmacy and primary care, these insiders say.
According to Jain, it's not as simple as it sounds. He think Haven won't make much progress in these areas without bringing in experts in these areas who can navigate the system and advocate for regulatory changes.
"You're going to need a mix of suits and hoodies," he said. "To change society you need people who both understand it, but with enough remove that they can be critical."
Pharmacy is particularly complex. Very few people in the world truly have a gauge on how the system fits together, and many of them are on the payroll for a company in the space with its own agenda. In the United States, the government doesn't negotiate the costs of drugs. So all of that falls on a complex web of for-profit companies, including the health plans.
But the pharmacy costs for employers are astronomical, representing about 20 to 25 percent of their overall health care spending, so it would be impossible to ignore for a group with Haven's goals. For that reason, it's not altogether surprising that the current COO hails from the world of pharmacy benefits.
Another crucial area in improving access to preventative and primary care -- Mitchell says we have to do that, "or we'll be overrun with monopolistic health care systems doing price gouging." Primary care, in her view, offers a way to avoid downstream costs by catching health issues before they get serious.
Having a relationship with a family doctor, whether it's online via telemedicine or in-person, can also be key to helping employees live healthier lives. And it can help reduce admission rates to the hospital, which are a huge cost driver for employers.
In Mitchell's view, there's a big moment now. Many employers are struggling during the pandemic, and are looking for ways to reduce their overhead
"These cost pressures could force change," she said. "For the right person at the helm, who understands health operations and knows what they're up against, there's a big opportunity here."